Fresh Approaches
Hope for Chronic Pain Relief Grows at UTD
By Stephen Fontenot
In an era of increased opioid-related addiction and deaths, the way we treat all pain patients is under the microscope.
From 2013 to 2016, the National Institutes of Health (NIH) spent more than $1.9 billion to fund pain research. At stake, the well-being of more than 25 million U.S. adults who in 2012 reported suffering from daily chronic pain — a subset of which is affected by the ongoing opioid crisis.
According to January 2018 data from the NIH, more than 90 Americans each day die after overdosing on opioids — prescription pain relievers, heroin and synthetic opioids like fentanyl. Between 21 and 29 percent of chronic-pain patients who are prescribed opioids misuse them, and 8 to 12 percent develop an opioid-use disorder.
Three University of Texas at Dallas scientists — Drs. Ted Price BS’97, Greg Dussor and Zach Campbell — are attacking this ever-present problem from varied angles, each with his own focus, background and motivation for understanding it, reducing it and pre-empting it.
Their work contributes to the broader landscape of efforts at improving the human condition for generations to come.
The Pain that Lingers
Dr. Ted Price knows pain in every sense of the word.
As a researcher, he has studied the signaling pathways in pain-sensing neurons for 15 years.
As an athlete, he has endured the aftereffects of a spinal injury, giving him insight no research paper could offer.
And as an advocate, he’s spoken with federal officials and worked with programs to address the opioid addiction epidemic plaguing our nation.
Price’s current quest is to find a permanent replacement for opioids — to find something that truly treats chronic neuropathic pain.
“Opioid use for chronic pain shouldn’t exist. The drugs don’t work,” says Price, a Fellow, Eugene McDermott Professor in the School of Behavioral and Brain Sciences. “But there’s no alternative, and I think physicians feel morally obligated to offer something.”
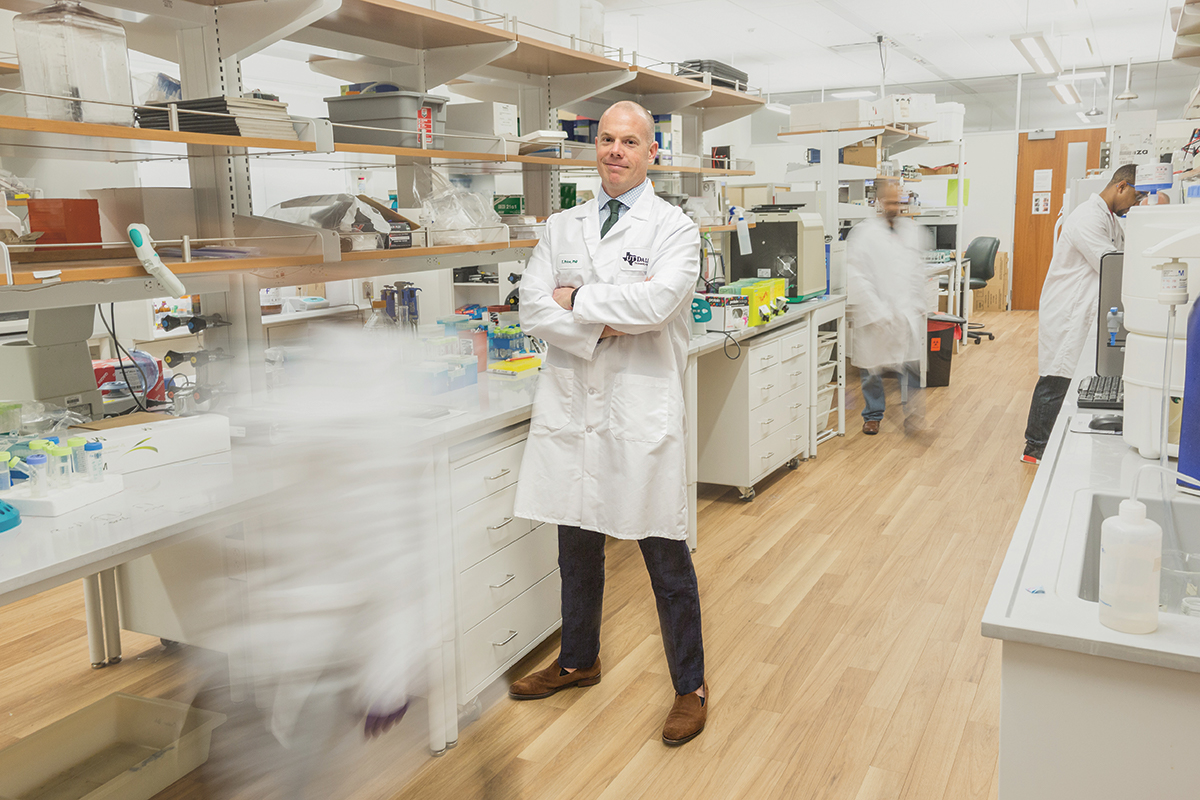 Dr. Ted Price co-chaired a work group for the Federal Pain Research Strategy.
Dr. Ted Price co-chaired a work group for the Federal Pain Research Strategy.
Price’s work on pain pathways began in 2003 at McGill University in Montreal. Four years later, he published a paper that made a large leap forward in the field.
“Lots of people started working on it then,” Price says. “I was on to something, and people were expanding the field.”
Price describes clinical pain as a situation where nerve cells, or neurons, become extraordinarily sensitive. He’s focused on the molecular signals that turn up the amplification. In 2011, Price published work identifying the AMP-activated protein kinase (AMP-K) enzyme as a negative regulator of that amplifier — it turns the knob back down.
“In the years since we’ve published, about 100 papers have been written confirming that AMP-K activators reduce pain,” he says.
Price advocates for repurposing existing medications and it just so happens that an omnipresent drug fits the bill for his project.
“We found that metformin, a drug used for Type 2 diabetes, has really strong effects as an AMP kinase activator,” Price says. “It is the most widely prescribed drug in the world. It’s very safe and very inexpensive.”
With momentum building toward a prospective clinical trial for metformin, Price describes himself as “extremely hopeful.”
“If we find something that suggests we could use metformin for pain associated with chemotherapy, that’s amazing,” he says. “That situation is becoming increasingly common. We could prevent a tremendous amount of suffering, then perhaps do more trials in other populations to increase the scope of these drugs.”
At the same time, Price has a backup plan. Through an NIH grant, CerSci Therapeutics — a company Price helped to form to find nonopioid pain solutions — is working on more potent AMP-K activators for treatment of post-surgical pain.
“There’s a stigma against people who have chronic pain. Many are accused of being drug addicts or drug seekers, which is completely unfair.”
“We want to replace opioid use. That’s when most people become addicted, through a prescription for acute pain related to surgery,” Price says. “Pharmaceutical company Merck studied long-term dosing of AMP-K activators and proved these compounds are safe. I think there’s a great chance these compounds can be approved for a variety of diseases.”
Regardless of the strength of the evidence, Price knows that supplanting opioids in the market will be a tough task.
“The oldest pain medicines humans have are aspirin, marijuana and opioids,” Price says. “Can we eliminate reliance on them in the short term? Probably not. It may be that there’s simply nothing better than opioids for acute pain — for the first 24 hours after surgery or a horrific injury. But we can do better after that.”
From his experience with advocacy on the issue, Price knows it’s a slow battle.
“It’s going to take a coordinated effort, and a lot of political will. But we’re now equipped with data on two major fronts that moves the needle,” he says. “We know now that using opioids for acute pain increases the incidence of chronic pain. Secondly, opioid use for chronic pain really doesn’t do anything, and probably makes people even worse.”
Price can speak on that topic from experience. In 2006, a degenerative disk he’d dealt with since he was 17 pushed into his spinal cord, causing intense, debilitating pain “so severe that I could see it — a bright red glow.”
“I thought that I knew what really severe pain was like. I didn’t,” he says. “I’m just flat-out lucky that it went away. I had surgery that had a 50/50 chance at working, and it did. I can’t imagine having a productive life with that. I can’t imagine my wife having a productive life with me being in that state.”
With that understanding came a sense of empathy.
“There’s a stigma against people who have chronic pain,” Price says. “Many are accused of being drug addicts or drug seekers, which is completely unfair.”
Though he was already studying neuropathy when his injury happened, Price says his plight did change his sense of urgency for the problem — and his interest in taking his quest beyond the laboratory. He’s been involved in federal programs on the opioid crisis, including as a co-chair on the Federal Pain Research Strategy’s work group on the transition from acute to chronic pain.
If he’s to leave his mark in this pursuit, Price knows his advocacy is as likely as his research to make the difference.
“It’s totally ridiculous to think that I’m going to be the one to solve this problem,” he says. “It’s going to be hundreds, if not thousands, of people working together. But somebody has to champion that. And I, along with a couple other people around the country, have put in a lot of effort to do that. And what happened to me had a big impact.”
Dr. Greg Dussor is chipping away at a task many researchers have declined to take on.
His pursuit is to improve our understanding of migraine — a condition defined by recurring, severe headaches and associated visual issues and nausea, believed to affect one in every seven people worldwide.
That’s a billion brains to care for, and the path to an effective treatment is long and poorly lit. Dussor was drawn to it for those reasons.
“I had a colleague at the University of Arizona who was doing work on migraine,” says Dussor, a Fellow, Eugene McDermott Professor in the School of Behavioral and Brain Sciences. “From conversations with him about the state of the field, what we know and don’t know, and how big a problem it was, it just became hard to ignore.”
“… with migraine — there’s a ton that we don’t know, and that tends to scare people away from doing work in this field.”
Dussor has spearheaded work on a protein called brain-derived neurotrophic factor (BDNF), a potential cause of hypersensitivity to pain in migraine sufferers.
Difficulty in treating migraine sufferers stems from several issues, including an inability to pinpoint concrete symptoms and the disease’s gender imbalance.
“When you can’t find the problem with a brain scan or blood test, when there’s no biomarker, it’s natural for the medical community to say, ‘I can’t see anything wrong with you,’” Dussor says. “Combine that with the fact that migraine is three times more common in women than in men — the medical community has failed to take it seriously. It wasn’t legitimized as a medical condition until the last few decades.”
The primary problem, though, is that the cause of a migraine simply hasn’t been determined.
“We don’t even know where a migraine comes from,” Dussor says. “With something like Parkinson’s disease, we know where the pathology is. We don’t know how it gets that way, and we don’t know how to fix it once it gets that way, but we know where the problem is. Not so with migraine — there’s a ton that we don’t know, and that tends to scare people away from doing work in this field.”
While most pain can be classified as either nociceptive — caused by damage to body tissue — or neuropathic — related to nerve damage — Dussor says migraine defies either description.
“It’s a completely dysfunctional pain state,” he says. “There’s nothing obvious driving it, and you can’t point to a single event or series of events — that we understand — and say ‘that’s where your migraine started.’”
Though migraine has several components beyond the pain, Dussor is focused on the element that matches his expertise — tackling the pain disorder.
“The first thing I ask is, ‘Where could the pain possibly be coming from?’” he says. “The brain is not sensitive to pain, but the meninges, the tissues that encase the brain and spinal cord, are heavily innervated with pain-sensing neurons. It makes sense that it would start there. But there’s no tumor, no stroke, no rupture — no evident cause.”
“You need a lot of people working on this from different angles.”
Simultaneously, other researchers attack the problem from a background of broader neurology, pursuing the symptoms that occur before the pain ever starts. Some people see an aura that indicates a headache is coming; others become disoriented or can’t stop yawning. Dussor hopes that the research efforts meet in the middle somewhere.
“You need a lot of people working on this from different angles,” he says. “This is too complicated for anyone to say, ‘It’s only this.’ It’s bigger than that. So as we try to model the headache component, we acknowledge our limitations. But if we ultimately come up with mechanisms that treat the headache phase and don’t treat the other phases of migraine, that is still a massive contribution. Patients will tell you it’s the pain that keeps them out of work.”
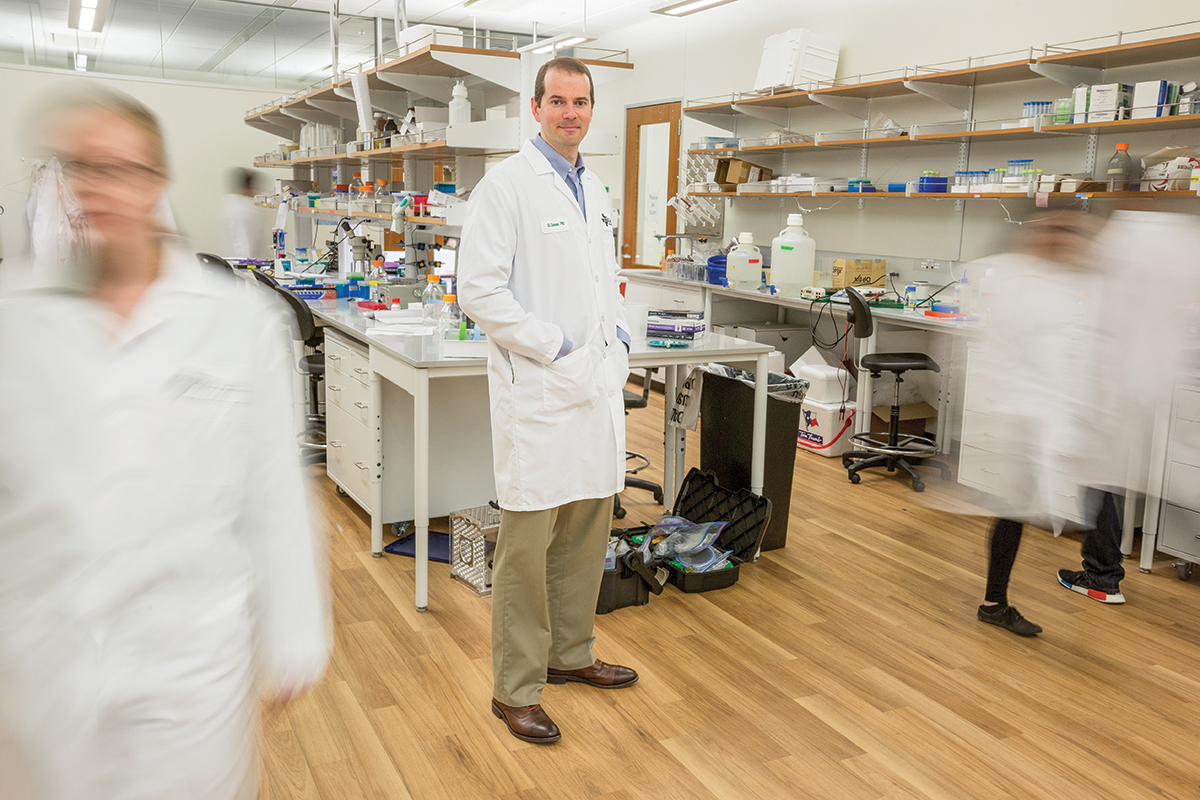 Neuroscientist Greg Dussor spearheads work on effective treatment of recurring migraine headaches.
Neuroscientist Greg Dussor spearheads work on effective treatment of recurring migraine headaches.
Another characteristic of migraine that cannot be ignored is its gender bias. Dussor explained that the pain-related differences between males and females could prove crucial, and he’s applying for new funding to explore this avenue of research.
“Our grant submission is based on the hormone prolactin and its role in migraine in females,” he says. “We hope to gain insight into why migraine is more common in women, and also develop ideas for therapeutics that may be female-specific.”
In a field that often seems far from a cure, it might seem easy to become discouraged. Dussor draws inspiration from the raw numbers of sufferers pulling for him and researchers like him.
“Anytime I give a talk, there’s always at least two or three people who will come up afterwards and just say, ‘thank you for the work you do,’” he says. “That’s the reward you get. This is an insanely common problem, but they know we’re trying to help.”
So Dussor beats on along an uphill path, knowing the goal at its end is worth the labor.
“In many respects, we’re in a very primitive phase of our understanding of migraine, and that needs to change,” he says. “It’s not going to change if people throw their hands up in the air and say this is a complicated thing, and we don’t want to do it. Somebody has to get on it.”
Dr. Zachary Campbell is still one of the new guys pursuing research at the Bioengineering and Sciences Building (BSB), but he’s quickly making his mark.
At his Laboratory of RNA Control, Campbell’s team has devised a way to block creation of the proteins that set pain in motion.
“We’re trying to block pathological protein synthesis where it happens,” says Campbell, an assistant professor of biological sciences in the School of Natural Sciences and Mathematics. “When you have an injury, certain molecules need to be made rapidly. Learning how that unfolds, we might be able to design pain medication that is by its nature nonaddictive — it won’t interact with the central nervous system because it acts where the injury is.”
Campbell’s approach intends to address both immediate and chronic pain — and in the process, give us a glance at how neurons “remember” pain.
“If I smash my hand with a hammer, for days after, even gentle touch is incredibly painful,” he says. “A month after, even a minor injury to that area feels like I just whacked myself with a hammer again — the neurons haven’t forgotten that original insult. These compounds block both the acute phase of pain and the longer-term memory.”
Campbell describes individual peripheral neurons — those outside the spinal cord and brain — as akin to partygoers in a crowded room.
“They can all hear one another and communicate in a coherent way. Then someone starts screaming incessantly and won’t quiet down,” says Campbell, describing hyperexcitability. “That ability to calm back down is what we think of as being the memory of a peripheral neuron. That’s the process I’m trying to affect.”
After an injury, instructions from the genome — the full genetic data present in each cell — are translated to create pain-signaling proteins. Those instructions are encoded in molecules called messenger RNA, or mRNA. Campbell’s team constructed a new class of decoy RNAs that interrupt the pain-protein synthesis process that mRNA facilitates, reducing signs of inflammation and impairing pain behaviors.
When injected at the site of an injury in experiments on mice, the decoy showed the ability to reduce behavioral response to pain.
“When the goal is overcoming nature, you’ve got to use whatever tools are available.”
“We’re manipulating one step of protein synthesis,” Campbell explained. “Our results indicate that local treatment with the decoy can prevent pain and inflammation brought about by a tissue injury.”
One huge hurdle in creating such an RNA-based compound was overcoming the rapid metabolism of these molecules.
“Molecules that degrade quickly in cells are not great drug candidates. The stability of our compounds is an order of magnitude greater than unmodified RNA,” Campbell says.
Campbell said that the project has vastly exceeded his wildest expectations for its first 18 months.
“It was kind of a risky, novel idea,” he says. “We now think we can get at RNA binding proteins, which make up 5 percent of the genome, with minor medications.”
The path of Campbell’s pain research has led him to pursue answers to some fundamental neurological questions.
“As I’ve gotten deeper into it, I’ve completely changed my perspective to asking, ‘If you have an injury, what changes?’ This gets at the molecular basis of memory itself,” he says. “In terms of the great questions in biology, if you can get close to touching ‘What is memory?’ what could be more remarkable than that? It’s one step removed from ‘What is consciousness?’ and I cannot imagine a more interesting problem than that.”
Campbell arrived at UT Dallas from the University of Wisconsin at Madison in 2015.
“There are several factors that were really important for me in coming here,” he says. “First, Ted and Greg have helped to create an amazing, fertile area for doing pain research.”
“The support that exists as a result of this building can’t be overlooked. It’s what physically joined all of our labs together.”
Secondly, Campbell emphasized that his work — and many similar projects originating at BSB — wouldn’t be possible without collaboration. And that is just what the designers of the building, which opened in 2016, had in mind when they included glass-walled labs and open spaces for formal and informal discussions among the bioengineers, neuroscientists, biologists and chemists who call it home.
“The real strength of UTD from my point of view has been its agility, which comes from groups of scientists willing to take a chance and work together,” he says. “The support that exists as a result of this building can’t be overlooked. It’s what physically joined all of our labs together.”
 Assistant Professor Zachary Campbell was drawn to UTD because of the research collaborations and outstanding facilities.
Assistant Professor Zachary Campbell was drawn to UTD because of the research collaborations and outstanding facilities.
Beyond the support of his colleagues, Campbell highlighted the role that the school’s funding of the core facilities plays. Core facilities are centralized research resources where various departments share the same technologies, services and spaces, encouraging interaction between diverse faculty members — a melting pot of innovation. Campbell credits Dr. Joe Pancrazio, a professor of bioengineering in the Erik Jonsson School of Engineering and Computer Science, with helping to bring core facilities to UT Dallas.
“UTD has hit critical mass. There’s been a ton of support from the administration,” Campbell says. “Core facilities were an incredible institutional leap, and in the context of pain research, it has allowed us to apply these cutting-edge genomics methodologies to study notoriously poorly understood problems. That’s been transformative for what I do.”
With that institutional support, Campbell envisions his pursuit eventually broadening to neurological targets beyond pain.
“I think if we understand what’s happening in the simplified neuronal system that relates to pain, we could get broadly useful insights for treating other types of neurophysiological diseases,” he says.
That effort has required repurposing some medications, creating other new pharmaceuticals, and designing new methodologies to validate experiments — all in a battle against the oldest foe.
“When the goal is overcoming nature, you’ve got to use whatever tools are at your disposal,” Campbell says.
Chronic Pain May Work Differently in Males and Females
Dr. Ted Price BS’97 and his colleagues in the Pain Neurobiology Research Group have produced a study supporting a hypothesis that chronic pain works very differently in males and females, perhaps heralding the creation of gender-specific painkillers.
A specific manipulation of receptors in the brain for the neurotransmitter dopamine impairs chronic pain generation in male mice but not in females. The results were published in the Journal of Neuroscience.
“For the same magnitude of pain in a male and a female, the mechanisms that drive pain seem to be remarkably separate,” Price says. “What we’re learning is that different types of cells drive the development of pain.”
The experiment focused on a newly discovered pain mechanism related to D5 dopamine receptors. Mice that were engineered to lack these receptors showed significantly reduced pain responses — but only the males.
“If we see the same results in human tissues,” Price says, “it will support the idea that you could make a D5 antagonist drug to treat pain in men.”
Such results may soon yield a new model for pain relief medication.
“It leads me to believe that it’s fairly likely we’ll want to make male- and female-specific drugs for chronic pain,” Price says. “If not that, we may need to develop diagnostics to look at an individual’s cell types, so we can tailor the therapeutic based on the underlying mechanism. Either way, when you take what everybody has done in the field, these differences are something that we have to pay very close attention to, and I feel like they are going to lead to the breakthrough we all really want.”
VNS Signals a Direct Approach
Dr. Robert Rennaker and his colleagues at the Texas Biomedical Device Center (TxBDC) target a different mechanism in their quest to reduce chronic pain.
The TxBDC team has designed a wireless implant that stimulates the vagus nerve — the longest, most complex cranial nerve — to help rewire the brain.
“Targeted plasticity therapy (TPT) involves stimulating the vagus nerve to release chemicals capable of reorganizing the brain in very specific ways,” says Rennaker, director of the center and Texas Instruments Distinguished Chair in Bioengineering. “By pairing sensory input or motor output movements with activation of the vagus nerve, we target pathways in the brain.”
The TPT approach would target pain generated by the central nervous system, not peripheral areas. A good example is phantom limb pain reported by amputees.
“If you lose your upper arm, you have a 58 percent chance of developing phantom limb pain,” says Rennaker, who also is head of the bioengineering department. “We think the cause, in most cases, is a lack of input from the missing limb. The part of the brain that processed that information is now passive. The regions of the body near that limb move into that part of the brain and cause it to expand and become hyperexcitable.”
 Dr. Robert Rennaker
Dr. Robert Rennaker
TPT could reduce hyperexcitability by pairing vagus nerve stimulation (VNS) with sensory inputs from other body parts. Functional MRIs show the hyperexcited parts of the brain and help scientists identify the inputs for the surrounding brain areas, allowing them to drive nearby input areas into the hyperexcited region.
“If the shoulder and face have moved into the part of the brain once associated with a missing hand, touch and heat stimulation of these other regions helps us move in and shrink that region down,” Rennaker says.
Trials are planned in spinal cord and multiple sclerosis patients, who suffer motor deficits and pain issues.
“Our first task is to get them where they can use their hands and legs,” he says. “As a follow-on study, we’d look at chronic pain.”
With the TxBDC technology, the full therapy cost for a patient could be limited to around $3,000 — a tenfold decrease from similar current technologies. Rennaker hopes this yields a radical change in clinical care and research.
“Companies sell the traditional implant for about $23,000, and that doesn’t account for the surgical cost,” he says. “Our solution is minimally invasive and cost-effective. I think this is really going to change how we approach neurological injuries and disease in the future.”